For years, Mohs micrographic surgery (MMS), more concisely known as Mohs surgery, has worn the unofficial mantle of “gold standard” for the treatment of the keratinocyte cancers, basal cell and cutaneous squamous cell carcinoma (BCC and cSCC). In this issue, Mark Teich, The Skin Cancer Foundation’s scientific director, interviews Mohs expert C. William Hanke, MD, discussing what makes Mohs surgery the optimal treatment for many skin cancer patients and how it has evolved and improved over the years. Dr. Hanke also sounds a note of caution about how Mohs can be overused, entailing greater costs in time and resources for simpler cases that don’t require it. For those not familiar with the Mohs technique, Dr. Hanke explains the basics, below.
Basics of Mohs Surgery
Mohs surgery gives you the highest cure rate and lowest recurrence rate of any skin cancer treatment, while preserving the maximum amount of normal tissue. In many cases it allows for less complex reconstructions and provides superior cosmesis.
| Lesion | Five-year cure rate with Mohs surgery | Five-year cure rate with standard excision |
|---|---|---|
| Primary BCC | 99% | 90% |
| Recurrent BCC | 94% | 83% |
| Primary cSCC | 97% | 92% |
| Recurrent cSCC | 90% | 77% |
Why such a difference in cure rates? The bottom line is, Mohs surgeons can evaluate 100 percent of the surgical margin compared with only about 1 percent using standard surgical excision. So, they are assured of locating nearly all residual cancer cells with Mohs, whereas standard excision amounts to an educated guessing game.
In standard excision, the tumor is excised with an extra margin of presumably healthy tissue. The wound is closed and the excised tissue is sent to the pathologist for review. The pathologist examines the tissue using standard vertical section pathology (i.e., “bread loafing”), which involves imprecise and minimal sampling of the surgical margin.
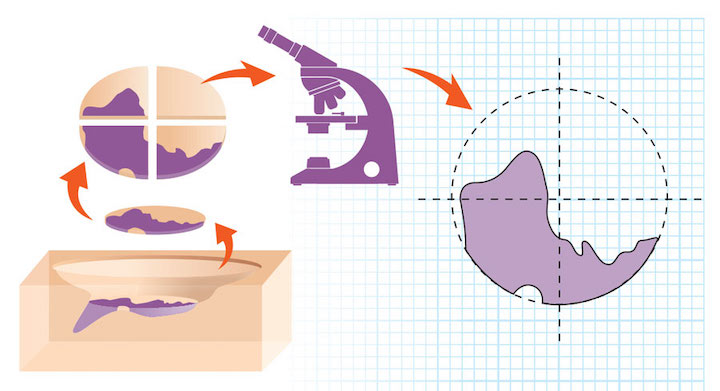
Mohs surgery involves quite a different process. Say there’s a marble-sized BCC on the nose. The Mohs surgeon first removes any gross tumor with a curette, then excises a layer of tissue with a very small peripheral margin of presumably healthy tissue. The surgeon color-codes this excised tissue and draws a precise map that correlates the tissue with the surgical site. The tissue is transported to the adjacent Mohs lab, where frozen sections prepared on a cryostat are sliced horizontally (like the layers of a layer cake rather than a slice from a loaf of bread). These sections encompass the complete deep and peripheral margins of the specimen, so the Mohs surgeon can thoroughly evaluate the interface between the patient and the excised tissue. The frozen sections are stained with histochemical stains that help differentiate normal from cancerous tissue. Then the Mohs surgeon evaluates the tissue under a microscope. One of the hallmarks of Mohs surgery is that the surgeon also functions as the pathologist, thereby eliminating unnecessary steps and reducing expenditure of medical resources.
If the Mohs surgeon identifies residual cancer cells microscopically, he or she knows exactly where they are located on the patient. The surgeon returns to the patient, who has been waiting in the office with a bandaged surgical site, and excises more tissue exactly where the tumor remains. The doctor repeats this process until the surgical site contains no microscopic evidence of tumor. The wound is then repaired or, in certain instances, allowed to heal on its own. The maximum amount of normal tissue has been preserved, so the repair can be minimized, resulting in a smaller, less noticeable scar.
The precise horizontal frozen sections utilized in Mohs surgery are much more difficult to prepare technically than standard vertical sections because the entire peripheral and deep margin of every specimen must be made visible. Mohs laboratory technicians are trained at a high level and have extensive experience.
Mohs surgeons have received training in surgery, pathology and reconstruction. Many have completed a one-year fellowship, working closely with an experienced Mohs surgeon to build a solid foundation. Generally, Mohs surgeons are a one-stop shop for skin cancer treatment and repair in the office surgical facility.
Mohs at Its Best: Optimal Usage
 C. William Hanke, MD, is a Mohs surgeon at the Laser & Skin Surgery Center in Indianapolis. A senior vice president of The Skin Cancer Foundation and a member of its Amonette Circle, he has served as president of 13 professional societies, including the American Academy of Dermatology, the American Society for Dermatologic Surgery, the American College of Mohs Surgery and the International Society for Dermatologic Surgery.
C. William Hanke, MD, is a Mohs surgeon at the Laser & Skin Surgery Center in Indianapolis. A senior vice president of The Skin Cancer Foundation and a member of its Amonette Circle, he has served as president of 13 professional societies, including the American Academy of Dermatology, the American Society for Dermatologic Surgery, the American College of Mohs Surgery and the International Society for Dermatologic Surgery.
Mark Teich: In what situations is Mohs surgery the best technique for keratinocyte carcinomas?
C. William Hanke, MD: In general, Mohs is the optimal technique for identifying and excising irregular microscopic extensions in basal cell carcinoma (BCC) and cutaneous squamous cell carcinoma (cSCC). It has an especially clear advantage over standard excision in critical anatomic areas such as the H-zone of the central face, where preserving normal tissue is essential for function and appearance. It should also be used for cSCCs that are problematic and associated with suboptimal outcomes using standard excision: those larger than 2 cm in diameter, those with tissue involvement below the subcutaneous fat and those with perineural invasion or poor differentiation.
In addition, Mohs should nearly always be considered for cSCCs and BCCs that have recurred following standard treatment. Because cSCC has a greater propensity to metastasize than BCC, complete microscopic removal of recurrent cSCC is extremely important. But Mohs should also be considered for recurrent BCC, which can cause considerable local tissue destruction.
As a general rule, we use Mohs in initial surgeries for primary BCCs and cSCCs in the H zone of the face and consider it for recurrent tumors in or outside of the H zone.
MT: What exactly is the H zone, and why is it so important to use Mohs in that area?
CWH: It’s essentially the central area of the face, which contains delicate structures that are important for function and cosmesis. For the eyelids, lips and nose, you want to preserve the maximum amount of normal tissue so that you can achieve the best functional and cosmetic result in closing the wound.
MT: Are there situations when you should not use Mohs?
CWH: In areas of the face or body where you have a small, localized tumor and no vital, delicate structures nearby, you could use another technique such as standard excision, curettage or cryosurgery. But even then, if you have a 1 cm or larger tumor, you may want to preserve and conserve as much tissue as possible, so Mohs might be called for.
Appropriate Use Criteria (AUC) for Mohs surgery have been jointly developed by the American Academy of Dermatology, American College of Mohs Surgery, American Society for Dermatologic Surgery and American Society for Mohs Surgery. These AUC criteria were published in JAMA Dermatology in 2012, delineating very specific indications for Mohs, and they remain the current standard. An update is underway and could be completed in the next two years.
Mohs surgeons like myself follow the Appropriate Use Criteria as much as possible, but there is leeway to go beyond. You don’t want to treat skin cancers with methods that are not cost-effective. Using Mohs for uncomplicated cancers can amount to overkill. Just because guidelines exist doesn’t guarantee that people will follow them, and there’s no law that says you have to follow them. However, as the technique gets overused and as costs to Medicare and private insurance go up, regulations on appropriate use will be implemented and enforced. We’re not at that point yet, but the current AUC criteria and their upcoming updates are a big step in the right direction.
Sometimes, other physicians and health-care providers refer patients to me for Mohs surgery when it is not indicated. When this occurs, it is important for the Mohs surgeon to explain to the referring physician and patient why other, non-Mohs treatments may be more appropriate.
MT: A recent study suggested that Mohs may even be a superior technique for superficial BCCs, producing higher cure rates than other techniques. When, if ever, would you consider it appropriate to use Mohs for superficial BCC or cSCC?
CWH: It’s true that Mohs surgery would provide high cure rates for superficial BCC and cSCC, but using Mohs routinely for superficial skin cancers in noncritical areas is like using an elephant gun to kill a squirrel. In general, it is not cost-effective and amounts to overtreatment. Other non-Mohs treatments should be sufficient to cure these tumors. The exceptions are recurrent BCCs and cSCCs; Mohs surgery nearly always should be a consideration for these tumors, even if they are superficial, especially in critical areas.
MT: What is your response to dermatopathologists who say it is better to work with fixed tissue specimens than the frozen sections Mohs surgeons generally use?
CWH: Permanent fixed tissue sections may have an advantage for dermatopathologists or pathologists who are focused on histopathologic diagnosis. Mohs surgeons, on the other hand, already know the diagnosis and are trying to remove the cancer. Dermatopathologists and general pathologists may spend their entire day looking at permanent sections, which take days to prepare, while frozen sections take half an hour to prepare while the patient waits. Most pathologists are impressed when they see the remarkable high quality of our frozen sections. The refinement of Mohs frozen section techniques has made them equal in quality to permanent sections.
MT: How else has Mohs surgery improved or evolved in recent years?
CWH: Super wide-field microscopes and automated staining have improved the efficiency of slide preparation and analysis. Most Mohs surgeons utilize hematoxylin and eosin (H&E) staining of frozen sections, but a minority use toluidine blue staining. Immunostains have added precision in differentiating normal tissue from tumors such as melanoma in situ as well as other uncommon malignancies that present analytic challenges, such as dermatofibrosarcoma protuberans (DFSP), sebaceous carcinoma, extramammary Paget’s disease, Merkel cell carcinoma and microcystic adnexal carcinoma.
It remains to be seen what role artificial intelligence and improved imaging will play in Mohs surgery. Preliminary studies with noninvasive imaging, i.e., optical coherence tomography (OCT) and multispectral optoacoustic tomography (MSOT), have been directed at Mohs surgery, but I do not believe that these technologies will replace precise Mohs frozen section histopathology anytime soon.

Désirée Ratner, MD
Editor-in-Chief, Carcinomas & Keratoses
Mohs for Melanoma
Our second issue of Carcinomas & Keratoses chiefly focuses on Mohs micrographic surgery (MMS) for the keratinocyte cancers, basal and cutaneous squamous cell carcinoma, which is its principal use in dermatology. It has not to date been as widely used for melanoma, since melanocytes until recently were hard to distinguish from keratinocytes on frozen sections. For decades, particularly in sun-damaged skin, the permanent sections used in standard excision were regarded as superior to the frozen sections used in Mohs surgery when evaluating melanoma specimens.
Thus, wide local excision (WLE) with permanent sections has been the standard for melanoma, with margins dictated by Breslow depth. However, in this technique less than 1 percent of the surgical margin is examined histopathologically, making it difficult to assess the extent of residual tumor. Furthermore, the true margins of melanomas, particularly larger lesions and those in sun-exposed areas, can extend well beyond their clinically detectable borders, increasing the risk of recurrence unless careful margin control is exercised.
Today, advances in immunohistochemistry (IHC) have made it much easier to detect melanocytes in frozen tissue using antibodies such as MART-1, MiTF and SOX10. With the recent advent of rapid staining protocols, neither time nor slide quality can still be considered a barrier to IHC evaluation of fresh frozen tissue. A growing body of evidence suggests that Mohs surgery with immunohistochemistry is safe and effective for both in situ and invasive melanoma.
Since MMS with IHC permits 100 percent margin assessment of excised tissue involved with malignant melanocytes, providing maximum visualization of any remaining cancer while sparing the greatest amount possible of histologically normal tissue, it should be especially useful for melanomas with indistinct borders or in high-risk areas. Ill-defined lesions can be removed with narrower margins yet immediate confirmation of histologic clearance, as can lesions of the head, neck, hands, feet and genitalia. The same is true for large or recurrent lesions, already considered appropriate indications for MMS in keratinocyte carcinomas.
The low recurrence rates and high survival rates reported using MMS with IHC for both melanoma in situ and invasive melanoma are encouraging; studies directly comparing WLE and MMS with IHC are now warranted to dispel any remaining questions or concerns.
Clinical Trial Alert
Patients who have Gorlin syndrome (also known as nevoid basal cell carcinoma syndrome) are genetically predisposed to developing multiple and recurrent BCCs, starting as early as adolescence. Some people with the rare syndrome develop hundreds or even thousands of these skin cancers. These patients usually undergo many treatments — including Mohs surgeries. PellePharm is sponsoring a phase 3 clinical trial to investigate patidegib, a topical hedgehog inhibitor for the reduction of the basal cell carcinoma burden in patients with Gorlin syndrome, while minimizing the side effects of oral hedgehog inhibitors. This trial will enroll approximately 150 patients with Gorlin syndrome at two dozen sites in the United States and Canada (gorlinstudy.com) and another two dozen sites in Europe. For details, see https://clinicaltrials.gov/ct2/show/NCT03703310
American College of Mohs Surgery: MohsCollege.org
American College of Mohs Surgery Surgeon Finder:
MohsCollege.org/surgeon-finder
The Skin Cancer Foundation’s Mohs surgery brochure, “Mohs Micrographic Surgery for Treating Skin Cancer.” Visit The Skin Cancer Foundation’s online store: store.SkinCancer.org